Abstract
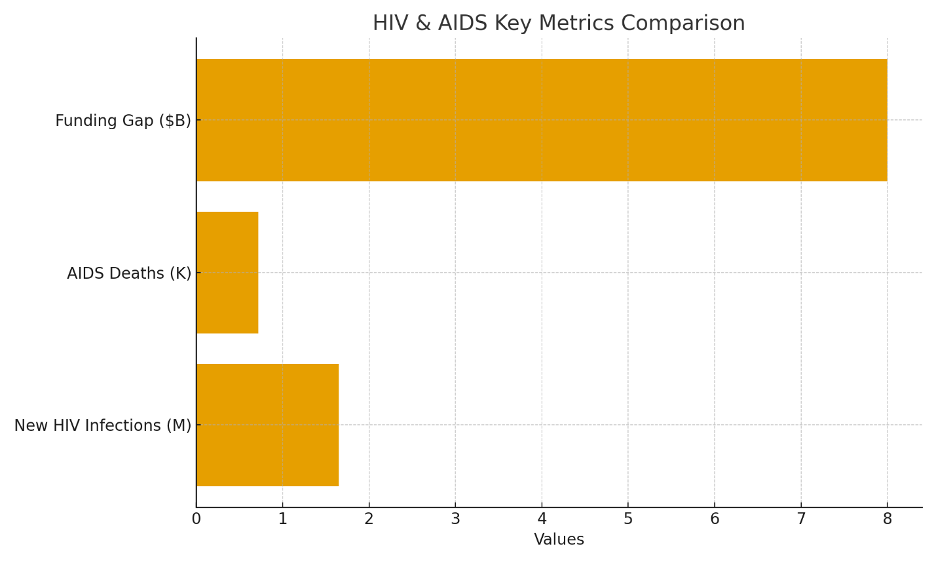
The human immunodeficiency virus (HIV) epidemic persists as a significant public health challenge in 2025, with approximately 39 million individuals living with HIV globally and 1.3 million new HIV infections reported in 2022. Despite substantial reductions in new infections (22% decline from 2010 to 2021) and AIDS-related deaths (40% decrease to 718,000), emerging epidemics in regions such as Asia-Pacific and low-prevalence areas outside sub-Saharan Africa threaten sustained progress. This article examines key epidemiological trends, the role of pre-exposure prophylaxis (PrEP), the undetectable equals untransmittable (U=U) principle, and viral suppression in achieving UNAIDS 95-95-95 targets (95% diagnosis, 95% treatment coverage, and 95% viral suppression). It analyzes contributions from organizations including PEPFAR and the Global Fund HIV, persistent barriers such as stigma and funding shortfalls, and evidence-based recommendations for policy and practice. Drawing on recent data from UNAIDS, WHO, and Global Burden of Disease studies, the analysis underscores the imperative for accelerated interventions to end AIDS as a public health threat by 2030.
Introduction
Since its identification over four decades ago, HIV has evolved from an acute fatal illness to a manageable chronic condition through advances in antiretroviral therapy (ART). In 2025, the global landscape reflects both achievements and vulnerabilities. New HIV infections decreased from 2.11 million in 2010 to 1.65 million in 2021, while AIDS deaths fell from over 1.2 million to 718,000. These gains align partially with UNAIDS 95-95-95 targets, which aim for 95% of people living with HIV (PLWH) to know their status, receive treatment, and achieve viral suppression by 2025. However, 1.3 million new infections in 2022 exceeded the target of fewer than 370,000 annually, highlighting implementation gaps.
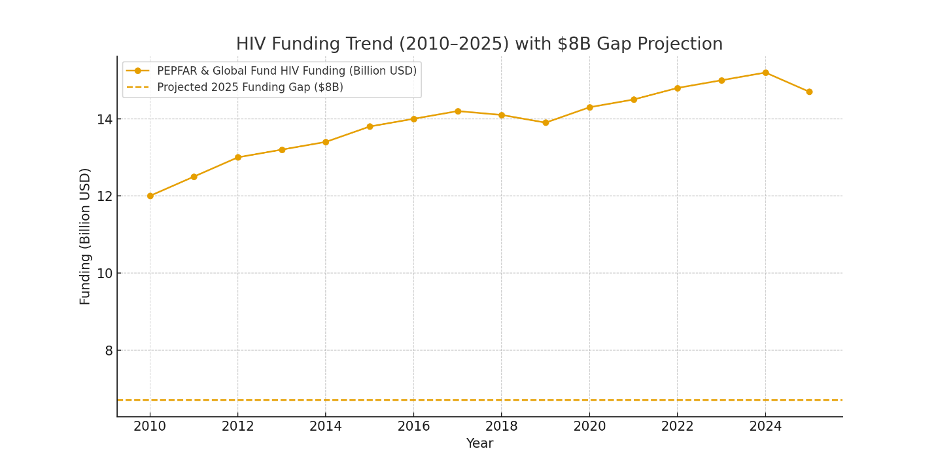
Sub-Saharan Africa bears 77% of new infections, disproportionately affecting adolescent girls and young women. Emerging hotspots, including the Philippines (57% case increase in Q1 2025) and low-prevalence regions, indicate shifting epidemiology. Funding constraints, exacerbated by PEPFAR suspensions and an $8 billion shortfall against a $29.3 billion annual need, compound risks. This review synthesizes 2025 data to evaluate progress, interventions, and barriers, employing a structured analysis informed by UNAIDS Global AIDS Update 2025 and Global Burden of Disease (GBD) studies.
Epidemiological Trends and Key Statistics
Global HIV prevalence stands at 39 million PLWH, with age-standardized incidence declining 41% since 1990, though overall prevalence rose 222% due to ART-extended survival. Table 1 presents ten critical indicators:

Core HIV/AIDS Indicators (2021-2025 Data)
| Indicator | Value/Trend |
| PLWH globally | 39 million |
| New HIV infections (2021) | 1.65 million |
| AIDS deaths (2021) | 718,000 (40% decline since 2010) |
| Diagnosis rate | 86% (target: 95%) |
| PrEP users targeted (2025) | 10 million |
| Viral suppression (U=U threshold) | 95% on ART |
| Annual funding requirement | $29.3 billion (gap: $8 billion) |
| Philippines Q1 2025 cases | 5,101 (57% increase) |
| Undiagnosed PLWH | 1 in 7 |
| Projected impact of targets | 90% AIDS death reduction by 2030 |
These metrics reveal stalled momentum: COVID-19 disruptions risked 10% more infections and 2.6 million additional cases by 2030. Sub-Saharan Africa HIV dominates, with 77% of incident cases among females aged 15-24, driven by structural factors including gender inequity and limited service access.
Interventions: PrEP, U=U, and Viral Suppression
Pre-exposure prophylaxis (PrEP) represents a cornerstone of prevention, reducing acquisition risk by 99% in high-adherence populations. Long-acting injectables address adherence barriers, targeting 10 million users by 2025. The U=U principle, grounded in epidemiological evidence, confirms zero transmission risk with sustained viral suppression (<200 copies/mL). Viral suppression via ART not only enhances individual health but interrupts transmission, aligning with treatment-as-prevention paradigms.
Progress varies regionally: Eastern and Southern Africa approach 95-95-95 (e.g., Malawi at 92-95-94), while Asia-Pacific lags. Join point regression analyses from GBD 2021 forecast stabilization with target attainment, but warn of reversals absent scale-up.
Organizational and Governmental Contributions
UNAIDS coordinates 95-95-95 implementation, modeling 32 million on ART and 90% mortality reductions via community-led delivery (30% of services). PEPFAR supports 77 high-burden countries, treating 20.6 million despite 2025 suspensions risking 630,000 additional AIDS deaths in sub-Saharan Africa. The Global Fund HIV mobilizes resources for diagnostics and ART in low-resource settings.
WHO emphasizes stigma reduction and adolescent-focused care; EU/EEA expands PrEP in 10 nations. National efforts, such as Philippines Department of Health surveillance and Ethiopia’s AI-driven forecasting, exemplify localized adaptation.
Barriers: Stigma, Funding, and Structural Inequities
Stigma impedes testing and retention, with 1 in 7 undiagnosed PLWH facilitating onward transmission. Systematic reviews identify healthcare discrimination as a key deterrent, necessitating interventions like anti-stigma training. PEPFAR funding volatility, influenced by U.S. policy shifts, threatens equity.
Structural determinants exacerbate disparities: sub-Saharan Africa’s gender dynamics yield three-fold higher incidence in young women; key populations (LGBTQ+, sex workers) face exclusion. Drug resistance and aging PLWH comorbidities (e.g., frailty in >50% over age 50 in high-income settings) demand integrated care.
Myths and Misconceptions: Evidence-Based Clarification
Debunks prevalent myths, supported by empirical data:
Myths vs. Evidence in HIV/AIDS
| Myth | Evidence-Based Fact |
| HIV/AIDS is invariably fatal | ART confers near-normal lifespan; U=U eliminates transmission with viral suppression |
| Visible symptoms identify HIV | Asymptomatic phase predominates; testing detects 86% of cases |
| Prevention is ineffective | PrEP/PEP avert 99% of exposures; condoms enhance efficacy |
| Absence of cure precludes control | Chronic management akin to diabetes achieves viral suppression |
Addressing these fosters uptake and reduces discrimination.
Future Projections and Research Priorities
UNAIDS Global AIDS Update 2025 projects epidemic control by 2030 with depoliticized funding and innovation (e.g., NYVAC vaccine vectors). GBD forecasts declining PLWH post-2023 under optimal scenarios, but warn of 2.6 million excess cases otherwise. Priorities include RCTs for stigma interventions, scalable PrEP in adolescents, and cyclical cascade models capturing care discontinuities.
Recommendations
- Scale community-led models to 30% of services, prioritizing key populations.
- Secure $29.3 billion annually via Global Fund replenishment and PEPFAR stabilization.
- Integrate mental health and NCD screening in HIV care.
- Deploy AI for outbreak prediction and adherence monitoring.
- Normalize U=U in public health campaigns to combat stigma.
Conclusion
The 2025 HIV landscape demonstrates resilience amid fragility. UNAIDS 95-95-95 targets offer a viable pathway to end AIDS by 2030, contingent on bridging funding gaps, dismantling stigma, and leveraging PrEP/U=U innovations. Sustained multilateral commitment is essential to translate epidemiological modeling into tangible reductions in new HIV infections and AIDS deaths.